About 30% of the people with epilepsy have refractory epilepsy and do not respond well to anti-epileptic drugs. Stichting Epilepsy Instellingen Nederland (SEIN) is a tertiary referral centre for epilepsy and many of the referred people have epileptic seizures that do not respond to first line anti-epileptic drug treatment. This may be due to – solitary or concurrent – non-epileptic seizures, a wrong epilepsy diagnosis or to resistance to anti-epileptic medication. Understanding the cause and triggers of seizures is essential for finding the best treatment. Failure of first line drugs urges trials of second line drug treatment, alternative therapies and epilepsy surgery. The latter needs optimal delineation of the epileptogenic brain tissue. Treatment of refractory epilepsy requires a broad-spectrum approach including psychosocial aspects and co-morbidities. This research priority studies causes and triggers of epileptic and non-epileptic seizures, treatment optimisation through new drug trials, alternative treatment options and epilepsy surgery with optimal focus localisation and understanding the effect of epilepsy on psychosocial functioning and co-morbidities.
Causes and facilitators of the development of epilepsy
Causes and facilitators of the development of epilepsy can be found during early development, for instance abnormal cortical development, genetics, psycho trauma at early infancy and later-on, like autoimmune encephalitis and tumours. Causes of epilepsy are being studied in collaboration with the Amsterdam UMC (child psychology and neuropathology), with the Erasmus UMC in Rotterdam (neuroinflammation) and the UMC Utrecht (genetics).
How triggers affect the brain
Seizures can be triggered by stress and other hormonal changes, light flashes, sleep deprivation and other triggers. SEIN studies how these triggers affect the physiology of the system and excitability of the brain.
Non-epileptic seizures
Non-epileptic seizures occur in people with and without epilepsy. We are studying the prevalence and how this evolves over time and relates to treatment, e.g. around epilepsy surgery.
Development of new drugs
SEIN aids the development of new drugs. Second line drugs are being tested in cohort studies, often in people with specific aetiologies like Dravet syndrome or Juvenile Myoclonic Epilepsy. Farmacogenetics enables patient-specific drug treatment.
Alternative treatment
Alternative treatment options studied include the use of cannabis in certain types of epilepsy, vagal nerve stimulation and psychological treatment for stress-related epilepsy.
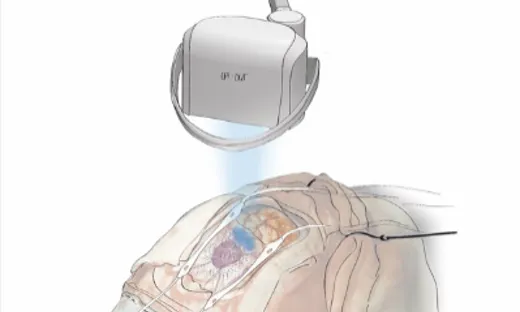
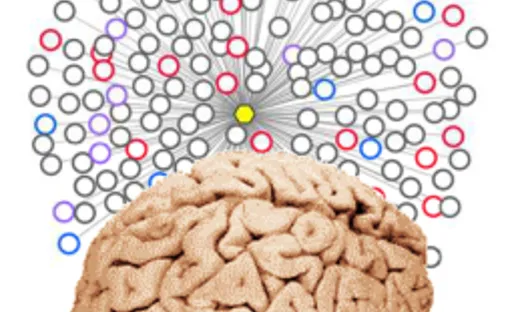
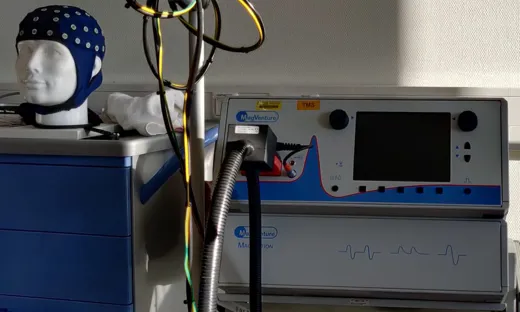
New technologies
The advancement of new technologies enable better understanding and focus localisation of epilepsy. Epilepsy surgery offers a potential cure for focal epilepsy. SEIN has an active presurgical work-up including video-EEG monitoring, MRI post processing, neuropsychological testing, nuclear imaging (PET/SPECT) and invasive EEG recording in collaboration with the UMC Utrecht. Focus localisation is being improved with MRI post-processing, multi-modal imaging, advanced (i)EEG signal analysis (modelling, networks, high frequency oscillations), MEG, TMS-EEG and intra-operative guidance.
Effect of epilepsy
The effect of epilepsy and seizures on psychosocial functioning and quality of life is large. SEIN offers dedicated treatment and guidance by (neuro) psychologists, social workers and other consultants and allows people with epilepsy to live in adapted environments. SEIN investigates home safety adjustments, automatic home seizure detection and the value of video monitoring of seizures.
Care
The care for people with refractory epilepsy is the core business of SEIN. This includes coping with the disease by patients and their caregivers, school, work, risk management and legal aspects.